The abducens nerve, also known as the sixth cranial nerve, plays a crucial role in eye movement. Assessing the abducens nerve is essential in diagnosing and managing conditions that affect its function. In this article, we will delve into the various aspects involved in the assessment of the abducens nerve, including its anatomy, function, clinical presentation, diagnostic techniques, interpretation of assessment results, treatment options, and prevention and management strategies for abducens nerve disorders.
Understanding the Abducens Nerve
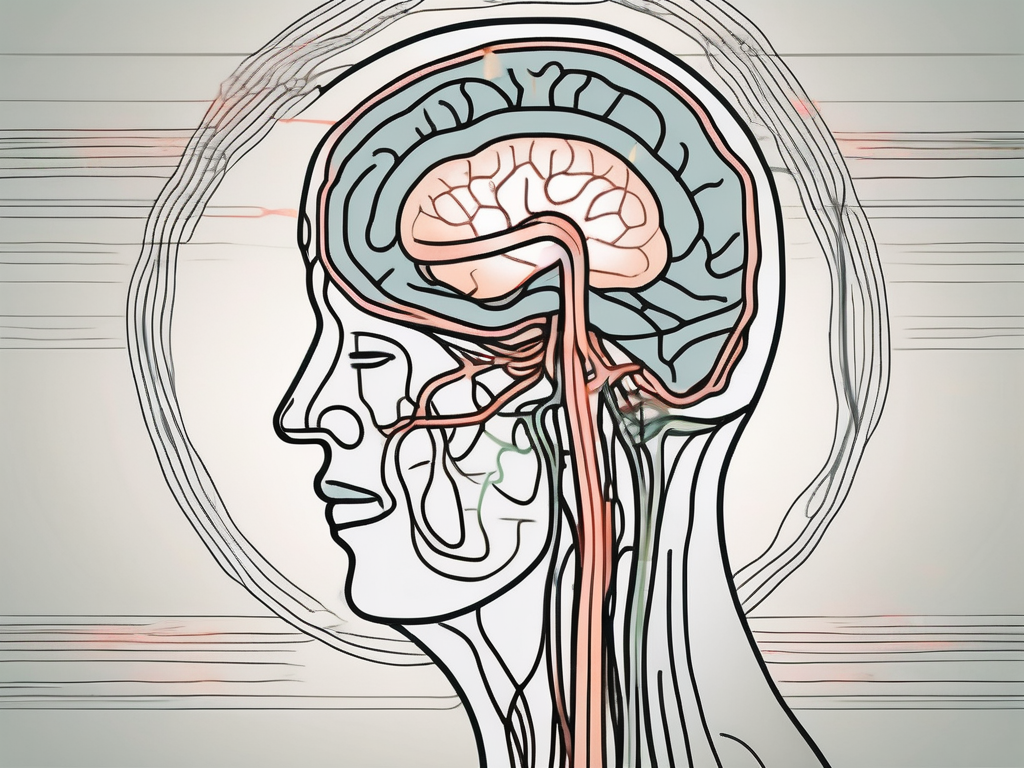
The abducens nerve is responsible for controlling the lateral rectus muscle, which aids in the outward movement of the eye. Located within the brainstem, this nerve originates in the pons region and traverses through the cavernous sinus before reaching the eye. Its intricate pathway makes it susceptible to various conditions that can impact its normal function.
Anatomy of the Abducens Nerve
The abducens nerve consists of a bundle of motor fibers originating from the abducens nucleus within the pons. These fibers course through the brainstem, exiting at the ponto-medullary junction, and then extend along the base of the skull before entering the cavernous sinus. From there, the nerve travels within the sinus and eventually reaches the lateral rectus muscle.
The abducens nerve’s pathway is not without its challenges. As it courses through the brainstem, it passes through a complex network of structures, including the pons and the ponto-medullary junction. This intricate journey exposes the nerve to potential compression or damage from surrounding structures, such as blood vessels or tumors. Additionally, the nerve’s passage through the cavernous sinus, a large venous structure located at the base of the skull, further adds to its vulnerability.
Within the cavernous sinus, the abducens nerve must navigate through a crowded space filled with other important structures, such as the internal carotid artery and other cranial nerves. This close proximity to vital structures increases the risk of compression or injury to the abducens nerve, leading to potential dysfunction.
Function of the Abducens Nerve
The primary function of the abducens nerve is to control the lateral rectus muscle, which allows for the movement of the eye away from the midline. This coordinated movement is essential for maintaining binocular vision and proper alignment of the eyes. Dysfunction of the abducens nerve can lead to impaired eye movement and subsequent visual disturbances.
When the abducens nerve is functioning properly, it works in harmony with the other cranial nerves and muscles of the eye to allow for smooth and coordinated eye movements. This intricate dance of nerve signals and muscle contractions allows us to explore our visual environment with ease and precision.
However, when the abducens nerve is affected by injury or disease, it can disrupt this delicate balance. Conditions such as abducens nerve palsy, where the nerve is unable to properly control the lateral rectus muscle, can result in a variety of symptoms, including double vision, eye misalignment, and difficulty moving the affected eye laterally.
Understanding the abducens nerve and its role in eye movement is crucial for diagnosing and treating conditions that affect its function. By studying the anatomy and function of this nerve, healthcare professionals can better comprehend the underlying causes of abducens nerve dysfunction and develop appropriate treatment strategies to restore normal eye movement and improve visual outcomes.
Importance of Assessing the Abducens Nerve
Assessing the abducens nerve is crucial for diagnosing and managing conditions that affect its function. By evaluating the integrity of this cranial nerve, healthcare professionals can identify abnormalities or palsy that may be indicative of underlying pathology.
The abducens nerve, also known as the sixth cranial nerve or cranial nerve VI, is responsible for the innervation of the lateral rectus muscle of the eye. This muscle is primarily responsible for the abduction of the eye, allowing it to move laterally away from the midline. Any dysfunction or impairment in the abducens nerve can lead to limitations in moving the eye laterally, resulting in a condition known as abducens nerve palsy.
Abducens nerve palsy can manifest in various ways, depending on the severity of the nerve dysfunction. Mild cases may cause only a slight limitation in eye movement, while severe cases can result in a complete inability to move the eye laterally. This can significantly impact a person’s ability to focus on objects located to the side, leading to difficulties in daily activities such as reading, driving, or even recognizing faces.
Role in Eye Movement
The abducens nerve plays a vital role in eye movement and coordination. It works in conjunction with other cranial nerves, such as the oculomotor nerve (cranial nerve III) and the trochlear nerve (cranial nerve IV), to ensure smooth and coordinated eye movements. When all these cranial nerves are functioning properly, the eyes can move in a synchronized manner, allowing for accurate tracking of objects and maintaining binocular vision.
Assessing the abducens nerve allows healthcare providers to identify potential causes of abducens nerve palsy and guide appropriate treatment measures. Common causes of abducens nerve palsy include trauma, infections, tumors, vascular disorders, and certain systemic conditions such as diabetes or hypertension. By thoroughly evaluating the abducens nerve, healthcare professionals can determine the underlying cause and develop a targeted treatment plan to address the specific pathology.
Connection to Neurological Disorders
Abducens nerve dysfunction can be associated with various neurological disorders, indicating the importance of assessing its function. Brainstem lesions, which can result from strokes, tumors, or demyelinating diseases, can affect the abducens nerve’s pathway and lead to palsy. In addition, increased intracranial pressure, commonly seen in conditions like hydrocephalus or brain tumors, can compress the abducens nerve and cause dysfunction.
Furthermore, abducens nerve dysfunction can be a sign of underlying systemic conditions such as multiple sclerosis or autoimmune disorders. These conditions can affect the nerves throughout the body, including the abducens nerve, leading to various neurological manifestations. By assessing the abducens nerve, healthcare professionals can decipher whether the dysfunction is isolated or part of a broader neurological issue, ultimately aiding in appropriate diagnosis and management.
In conclusion, assessing the abducens nerve is of utmost importance in the field of healthcare. By evaluating its function, healthcare professionals can identify abnormalities or palsy that may be indicative of underlying pathology. The abducens nerve’s role in eye movement and its connection to various neurological disorders highlight the significance of thorough assessment and prompt intervention to ensure optimal patient care.
Clinical Presentation of Abducens Nerve Palsy
Abducens nerve palsy commonly presents with distinct symptoms that clinicians should be aware of to facilitate accurate assessment.
Abducens nerve palsy is a condition that affects the sixth cranial nerve, also known as the abducens nerve. This nerve controls the movement of the lateral rectus muscle, which is responsible for moving the eye outward. When the abducens nerve is damaged or impaired, it can result in a variety of symptoms that can significantly impact a person’s vision and overall quality of life.
Symptoms to Look For
Individuals with abducens nerve palsy often complain of diplopia (double vision), which worsens when looking towards the affected side. This occurs because the lateral rectus muscle is unable to properly move the eye outward, causing misalignment of the eyes. As a result, the brain receives conflicting visual information, leading to double vision.
In addition to diplopia, patients with abducens nerve palsy also experience limitations in lateral eye movement. They may have difficulty looking towards the affected side, as the impaired abducens nerve prevents the eye from moving outward as it should. This limitation in eye movement can be frustrating and can affect a person’s ability to perform daily activities that require visual tracking.
It is crucial for clinicians to thoroughly evaluate these symptoms when assessing a patient with suspected abducens nerve palsy. A meticulous ocular examination should be performed, including assessing the alignment of the eyes, measuring eye movements in different directions, and evaluating visual acuity. Additionally, considering the patient’s medical history is essential, as certain underlying conditions or factors may contribute to the development of abducens nerve palsy.
Common Causes of Abducens Nerve Palsy
There are several factors that can lead to abducens nerve palsy. Trauma, such as head injuries or fractures of the skull, can damage the abducens nerve and result in its dysfunction. Intracranial lesions, such as tumors or aneurysms, can also compress or disrupt the nerve, leading to palsy.
Vascular abnormalities, such as aneurysms or arteriovenous malformations, can cause ischemia or bleeding in the area of the abducens nerve, leading to its dysfunction. Inflammation, such as that seen in conditions like meningitis or autoimmune disorders, can also affect the nerve and result in palsy.
In some cases, the cause of abducens nerve palsy may be idiopathic, meaning it is unknown. This can make diagnosis and management more challenging, as the underlying cause cannot be identified. However, even in these cases, thorough evaluation and consideration of potential contributing factors are crucial for formulating an appropriate management plan.
Diagnostic Techniques for Abducens Nerve Assessment
The assessment of the abducens nerve relies on a comprehensive approach, involving both physical examination procedures and imaging techniques.
When it comes to physical examination procedures, there are several key techniques that healthcare professionals employ to assess the function of the abducens nerve. A thorough ocular examination is essential in this process. It involves evaluating eye movements, assessing the pupillary response, and performing visual acuity tests. By carefully observing the patient’s eye movements, doctors can determine if there are any abnormalities or limitations in the lateral movement of the eye, which is controlled by the abducens nerve. The pupillary response is also examined, as abnormalities in this area can indicate dysfunction of the nerve. Additionally, specialized tests like the Hirschberg test and the cover test can provide valuable information about the alignment of the eyes and any associated muscle weakness.
While physical examination procedures can provide valuable insights, there are instances where further investigation is necessary. This is where imaging techniques come into play. In some cases, imaging studies may be warranted to further assess the abducens nerve or identify potential underlying pathology. One commonly used imaging modality is magnetic resonance imaging (MRI). This non-invasive procedure allows healthcare professionals to visualize the brainstem, cranial nerves, and surrounding structures with great detail. MRI is especially valuable when investigating suspected tumors, vascular abnormalities, or inflammatory conditions that may be affecting the abducens nerve. By obtaining high-resolution images, doctors can accurately assess the anatomy and function of the nerve, aiding in diagnosis and treatment planning.
In conclusion, the assessment of the abducens nerve involves a combination of physical examination procedures and imaging techniques. Through a thorough ocular examination, healthcare professionals can evaluate eye movements, pupillary response, and visual acuity. Specialized tests like the Hirschberg test and the cover test provide additional information about eye alignment and muscle weakness. In cases where further investigation is necessary, imaging techniques such as MRI can provide detailed images of the brainstem, cranial nerves, and surrounding structures. These diagnostic techniques play a crucial role in identifying abnormalities or pathology related to the abducens nerve, ultimately guiding appropriate treatment strategies.
Interpretation of Assessment Results
Interpreting the assessment results is crucial in determining the integrity of the abducens nerve and the underlying cause of any observed dysfunction.
The abducens nerve, also known as cranial nerve VI, plays a vital role in eye movement. It innervates the lateral rectus muscle, which is responsible for the abduction of the eye, allowing it to move laterally. When the abducens nerve functions optimally, it enables proper lateral eye movement and coordinated visual perception.
In a healthy individual, the abducens nerve carries out its function seamlessly, facilitating smooth eye movements and ensuring visual stability. However, when there are aberrations in abducens nerve function, various symptoms may arise. These symptoms can include limited eye movement, difficulty in moving the eye laterally, or even double vision.
Normal vs. Abnormal Findings
Interpreting the assessment results, along with correlating clinical findings, helps healthcare professionals differentiate between normal and abnormal presentations of abducens nerve function. By carefully analyzing the assessment outcomes, healthcare providers can gain valuable insights into the integrity of the nerve and identify any potential underlying causes for dysfunction.
During the assessment, various tests may be conducted to evaluate the abducens nerve. These tests can include assessing eye movements in different directions, examining the alignment of the eyes, and observing for any signs of nystagmus, which is an involuntary rhythmic movement of the eyes.
When the abducens nerve is functioning normally, the eye movements will be smooth, coordinated, and symmetrical. However, if there is damage or dysfunction present, the eye movements may be limited, jerky, or asymmetrical.
It is important to note that abnormal findings in the assessment results do not provide a definitive diagnosis. Instead, they serve as valuable indicators that further investigation is required to determine the underlying cause of the abducens nerve dysfunction.
Implications of Abducens Nerve Damage
Damage to the abducens nerve can have significant implications for individuals, affecting their overall quality of life and ability to perform daily activities. The severity of the damage and the specific symptoms experienced can vary depending on the underlying cause and the extent of the nerve injury.
Individuals with abducens nerve damage may experience difficulties in moving their eyes laterally, leading to a limited field of vision. This can impact their ability to navigate their surroundings, drive safely, or engage in activities that require precise eye movements, such as reading or playing sports.
Double vision, also known as diplopia, is another common symptom associated with abducens nerve damage. This occurs when the eyes are unable to align properly, resulting in the perception of two overlapping images. Double vision can significantly impact visual perception, making it challenging to perform tasks that require depth perception, such as judging distances or catching a ball.
Understanding the extent of the damage and the potential for recovery is essential in guiding appropriate treatment options and supportive measures. In some cases, abducens nerve damage may be temporary and resolve with time and proper management. However, in more severe cases, interventions such as surgery or vision therapy may be necessary to improve eye movement and restore visual function.
Additionally, healthcare professionals may recommend supportive measures to help individuals cope with the challenges associated with abducens nerve damage. These measures can include the use of prism glasses to correct double vision, occupational therapy to enhance daily living skills, and counseling to address any emotional or psychological impact resulting from the visual impairment.
Overall, interpreting the assessment results and understanding the implications of abducens nerve damage are crucial steps in providing appropriate care and support for individuals experiencing dysfunction in this important cranial nerve.
Treatment Options for Abducens Nerve Palsy
The management of abducens nerve palsy depends on various factors, including the underlying cause and the severity of symptoms.
Non-Surgical Interventions
In cases where abducens nerve palsy is secondary to an underlying condition, treating the underlying cause may lead to resolution of the symptoms. Additionally, optical aids such as prisms can help alleviate diplopia and improve visual perception. Consultation with an ophthalmologist and a neurologist is vital to determine the most appropriate treatment approach.
Surgical Procedures
When abducens nerve palsy does not respond to conservative measures or when there is evidence of significant nerve damage, surgical intervention may be considered. Strabismus surgery, for instance, can help to realign the eyes and improve binocular visual function. Surgical options should be discussed thoroughly with a specialist to weigh the potential risks and benefits.
Prevention and Management of Abducens Nerve Disorders
Preventing and managing abducens nerve disorders involves a multifaceted approach aimed at preserving and optimizing overall ocular health.
Lifestyle Modifications
Adopting a healthy lifestyle that includes regular exercise, a balanced diet, and adequate rest can contribute to overall eye health and minimize the risk of developing abducens nerve disorders. Avoiding excessive straining of the eyes and maintaining proper ergonomics when using digital devices can also help reduce the risk of ocular fatigue.
Regular Check-ups and Monitoring
Regular check-ups with an eye care specialist can aid in the early detection of potential abducens nerve disorders or any other ocular abnormalities. Routine evaluations can contribute to timely intervention and management, maximizing the chances of successful outcomes.
In conclusion, assessing the abducens nerve is crucial in determining its function, diagnosing related disorders, and guiding appropriate management strategies. Through a comprehensive evaluation that includes physical examination procedures and imaging techniques, healthcare professionals can identify abnormalities and formulate individualized treatment plans. It is important, however, to consult with a doctor or a specialist for professional medical advice tailored to one’s specific condition. Early intervention, accurate assessment, and proactive management contribute to optimizing ocular health and overall well-being.
Leave a Reply