The abducens nerve is a crucial component of the intricate neural network responsible for eye movement. Understanding its anatomy, function, pathway, and its role in various disorders is essential for medical professionals and researchers in the field of neurology. In this article, we will delve deep into the abducens nerve—examining its termination point, its pathway, and its associated disorders. Additionally, we will explore recent advancements in this area of study and their potential implications for future treatment options.
Understanding the Abducens Nerve
The abducens nerve, formally known as cranial nerve VI, is one of twelve cranial nerves originating from the brainstem. This nerve plays a pivotal role in controlling the lateral rectus muscle, which is responsible for the abduction movement of the eye. Its proper functioning is vital for coordinated eye movements and visual synchronization.
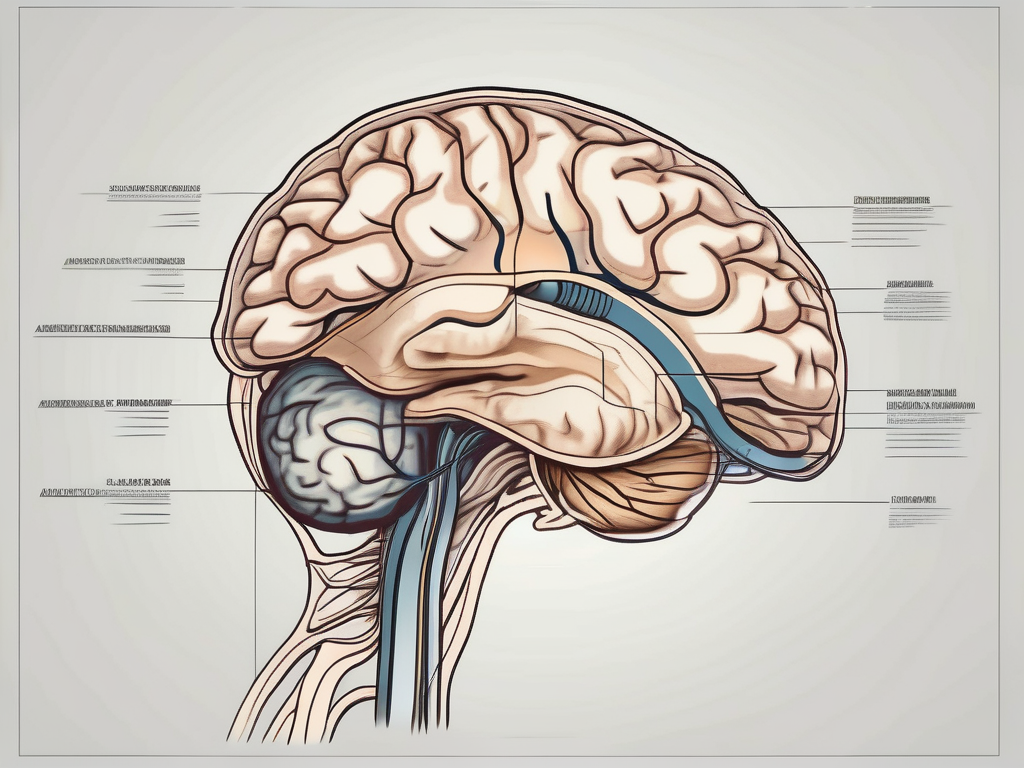
The abducens nerve, like other cranial nerves, has a fascinating anatomical structure. It emerges from the pons, a region of the brainstem located between the medulla oblongata and the midbrain. This nerve then descends through the cavernous sinus, a cavity in the skull that contains various blood vessels and nerves.
As the abducens nerve continues its journey, it traverses the superior orbital fissure, a narrow opening in the bony orbit of the eye. This anatomical pathway allows the nerve to reach its final destination: the lateral rectus muscle. The lateral rectus muscle is one of the six extraocular muscles responsible for moving the eye in different directions.
Due to its close proximity to neighboring cranial nerves and blood vessels, any pathological alterations can potentially result in dysfunction. In some cases, the abducens nerve can be affected by conditions such as tumors, trauma, or inflammation, leading to impaired eye movement and coordination.
Anatomy of the Abducens Nerve
The abducens nerve, being a crucial component of the ocular motor system, has a complex anatomy that warrants further exploration. It consists of both motor and sensory fibers, allowing it to transmit signals between the brain and the lateral rectus muscle.
The motor fibers within the abducens nerve originate from the abducens nucleus, a nucleus located in the pons. These fibers travel along the nerve pathway, eventually reaching the lateral rectus muscle. Once they reach their destination, they innervate the muscle, enabling it to contract and produce the necessary eye movement.
In addition to motor fibers, the abducens nerve also contains sensory fibers that provide feedback to the brain. These sensory fibers play a role in proprioception, which is the body’s ability to sense its position and movement in space. They relay information about the position and tension of the lateral rectus muscle, allowing the brain to maintain precise control over eye movements.
Function of the Abducens Nerve
The abducens nerve primarily facilitates horizontal eye movement, allowing the eye to move outward away from the midline of the face. This movement, known as abduction, is essential for visual exploration of the environment and maintaining binocular vision.
When the abducens nerve functions properly, it coordinates with other ocular motor nerves, such as the oculomotor and trochlear nerves, to ensure precise eye coordination. This coordination is crucial for activities that require accurate eye movements, such as reading, tracking moving objects, and maintaining visual fixation.
However, dysfunction of the abducens nerve can lead to various visual disturbances. One common symptom is diplopia, also known as double vision. This occurs when the eyes are unable to align properly, resulting in two overlapping images. Additionally, individuals with abducens nerve dysfunction may experience difficulty in rotating the eye outwards, limiting their ability to look towards the side.
Understanding the abducens nerve and its role in eye movement provides valuable insights into the complex mechanisms that govern our vision. Through its intricate anatomy and precise function, this nerve contributes to the remarkable coordination and synchronization of our eyes, allowing us to perceive the world around us with clarity and depth.
The Pathway of the Abducens Nerve
The journey of the abducens nerve begins with its origin and progresses through its course, playing a vital role in the transmission of signals for oculomotor control.
The abducens nerve, also known as cranial nerve VI, is responsible for the innervation of the lateral rectus muscle, which controls the movement of the eye laterally. Let’s explore the origin and course of this important nerve in more detail.
Origin of the Abducens Nerve
The abducens nerve originates from the abducens nucleus, situated in the pons region of the brainstem. This nucleus integrates signals from various regions of the brain, including the frontal eye fields and the oculomotor centers, and relays them to the lateral rectus muscle, enabling the desired eye movements.
Located close to the midline of the brainstem, the abducens nucleus receives input from both hemispheres of the brain, allowing for coordinated eye movements. It is fascinating to think about the intricate connections and communication between different regions of the brain that are involved in this process.
Course of the Abducens Nerve
After leaving the abducens nucleus, the nerve exits the brainstem and travels through the cavernous sinus, a cavity located on each side of the sella turcica, a bony structure in the skull. In this complex pathway, the abducens nerve joins forces with other important structures like blood vessels and cranial nerves.
As the nerve continues its journey, it passes through the superior orbital fissure, a narrow opening in the skull located between the greater and lesser wings of the sphenoid bone. This anatomical landmark is crucial as it serves as a gateway for the abducens nerve to reach its final destination.
Finally, after traversing through the superior orbital fissure, the abducens nerve reaches the lateral rectus muscle. This muscle, located on the outer side of the eye, contracts when stimulated by the abducens nerve, causing the eye to move laterally. It is remarkable to think about the precision and coordination required for this simple yet essential eye movement.
In conclusion, the pathway of the abducens nerve is a fascinating journey that begins in the abducens nucleus and progresses through the brainstem, cavernous sinus, and superior orbital fissure before reaching its target, the lateral rectus muscle. This nerve’s role in oculomotor control highlights the intricate connections and communication within the brain, allowing for precise eye movements. Understanding the pathway of the abducens nerve provides a glimpse into the complexity of the human nervous system and the remarkable mechanisms that govern our everyday actions.
Termination Point of the Abducens Nerve
The abducens nerve’s final destination is the lateral rectus muscle, where it terminates to exert control over this crucial component of eye movement.
The abducens nerve, also known as the sixth cranial nerve, is a vital player in the complex system that governs our eye movements. It originates from the pons, a part of the brainstem, and travels a long and intricate path before reaching its termination point at the lateral rectus muscle.
The lateral rectus muscle is one of the six extraocular muscles responsible for moving the eye. It is located on the outer side of the eye and is primarily responsible for abduction, which is the outward movement of the eye. Without the abducens nerve’s control over the lateral rectus muscle, our eyes would not be able to move laterally, limiting our ability to explore our visual surroundings.
Interaction with Other Nerves
The abducens nerve interacts with other cranial nerves, such as the oculomotor nerve and the trochlear nerve, to ensure coordinated and synchronized eye movement. This intricate collaboration among various neural pathways highlights the complexity of ocular motor control.
The oculomotor nerve, also known as the third cranial nerve, controls the majority of the eye’s movements, including the superior, inferior, and medial rectus muscles. It works in conjunction with the abducens nerve to ensure precise and coordinated eye movements in all directions.
The trochlear nerve, the fourth cranial nerve, controls the superior oblique muscle, which plays a crucial role in eye movements that involve a downward and inward rotation. The abducens nerve’s interaction with the trochlear nerve helps maintain the balance and synergy required for smooth and accurate eye movements.
Together, these cranial nerves form a complex network that orchestrates the intricate dance of eye movements, allowing us to explore our visual environment with precision and efficiency.
Role in Eye Movement
As mentioned earlier, the abducens nerve’s primary function is to control the lateral rectus muscle, enabling abduction—the outward movement—of the eye. This crucial role ensures that both eyes work in unison, allowing us to focus on objects efficiently and perceive depth accurately.
Eye movements are essential for various visual tasks, such as tracking moving objects, shifting our gaze between different points of interest, and maintaining binocular vision. The abducens nerve’s precise control over the lateral rectus muscle is crucial for these tasks, as it allows our eyes to move smoothly and accurately in response to visual stimuli.
Imagine trying to follow a fast-moving object without the abducens nerve’s control over the lateral rectus muscle. Our eyes would struggle to keep up, resulting in jerky and inefficient movements. The abducens nerve ensures that our eye movements are precise, coordinated, and effortless, contributing to our overall visual experience.
Furthermore, the abducens nerve’s role in eye movement extends beyond simple visual tracking. It also plays a crucial role in maintaining the alignment of both eyes, known as binocular vision. By controlling the lateral rectus muscle, the abducens nerve ensures that both eyes move together, allowing us to perceive depth accurately and have a three-dimensional visual experience.
In summary, the termination point of the abducens nerve at the lateral rectus muscle marks the culmination of a complex neural pathway responsible for controlling eye movements. Its interaction with other cranial nerves and its role in eye movement highlight the intricate and fascinating nature of ocular motor control.
Disorders Related to the Abducens Nerve
Although the abducens nerve performs its functions with remarkable precision, various disorders can disrupt its optimal performance. Understanding the symptoms, treatment options, and recovery possibilities associated with abducens nerve damage is crucial for patient care and management.
The abducens nerve, also known as the sixth cranial nerve, plays a vital role in eye movement. It is responsible for controlling the lateral rectus muscle, which allows the eye to move outward. When this nerve is damaged, it can lead to a range of debilitating symptoms that can significantly impact a person’s quality of life.
Symptoms of Abducens Nerve Damage
Damage to the abducens nerve can result in several pronounced symptoms, including diplopia (double vision), nystagmus (involuntary eye movements), and difficulty moving the eye laterally. These symptoms can vary in intensity, with severity depending on the extent of nerve damage.
Diplopia, or double vision, occurs when the abducens nerve is unable to properly coordinate the movement of both eyes. This can lead to a person perceiving two separate images instead of a single, clear image. Nystagmus, on the other hand, causes the eyes to make repetitive, uncontrolled movements, which can be disorienting and make it challenging to focus on objects.
In addition to these primary symptoms, abducens nerve damage can also cause eye fatigue, headaches, and difficulty reading or performing tasks that require precise eye movements. These secondary symptoms can further impact a person’s daily activities and overall well-being.
Treatment and Recovery Options
When faced with abducens nerve damage, it is essential to consult with a medical professional knowledgeable in neurology. Treatment options will depend on the underlying cause of the nerve dysfunction. Some cases may require conservative management, while others may necessitate surgical intervention or the involvement of a multidisciplinary team. Early diagnosis and appropriate intervention can contribute significantly to the chances of recovery.
In cases where the abducens nerve damage is caused by trauma or inflammation, non-surgical treatments such as medication, physical therapy, and eye exercises may be recommended. These interventions aim to reduce inflammation, improve nerve function, and enhance eye muscle coordination.
However, in more severe cases, surgical intervention may be necessary. Surgical options can include procedures to repair or bypass the damaged nerve, or even muscle transposition surgeries to improve eye movement and alignment. The decision to undergo surgery will depend on various factors, including the individual’s overall health, the extent of nerve damage, and the potential risks and benefits of the procedure.
Recovery from abducens nerve damage can vary from person to person. Some individuals may experience a complete resolution of symptoms over time, while others may have residual eye movement difficulties. Rehabilitation programs, including vision therapy and occupational therapy, can play a crucial role in maximizing recovery and helping individuals regain their independence.
It is important to note that the prognosis for abducens nerve damage depends on several factors, including the underlying cause, the extent of nerve damage, and the individual’s overall health. Regular follow-up appointments with healthcare professionals specializing in neurology and ophthalmology are essential to monitor progress and adjust treatment plans as needed.
Recent Research on the Abducens Nerve
Advancements in the field of neurology continue to shed light on the abducens nerve and its intricate interactions within the ocular motor system. These breakthroughs have promising implications for improved diagnostic techniques, novel treatment strategies, and a deeper understanding of complex neural networks.
The abducens nerve, also known as the sixth cranial nerve, plays a crucial role in eye movement. It innervates the lateral rectus muscle, which is responsible for the abduction of the eye, allowing it to move laterally. Dysfunction of the abducens nerve can lead to a condition called abducens nerve palsy, characterized by the inability to move the affected eye outward.
Advances in Neurology
Researchers have made significant progress in unraveling the underlying mechanisms and pathologies associated with abducens nerve disorders. Cutting-edge imaging technologies, such as magnetic resonance imaging (MRI) and diffusion tensor imaging (DTI), provide detailed anatomical and functional insights, aiding in both diagnostics and treatment planning.
MRI scans allow clinicians to visualize the abducens nerve and surrounding structures with remarkable precision. This non-invasive imaging technique uses strong magnetic fields and radio waves to generate detailed images of the brain and cranial nerves. By examining the size, shape, and integrity of the abducens nerve, neurologists can identify any abnormalities or lesions that may be causing dysfunction.
DTI, on the other hand, is a specialized MRI technique that measures the diffusion of water molecules within the brain’s white matter tracts. This imaging modality provides information about the structural integrity and connectivity of the abducens nerve fibers. By analyzing the direction and magnitude of water diffusion, researchers can map the neural pathways associated with the abducens nerve and better understand how they are affected in various disorders.
Future Implications for Treatment
The advancements in understanding the abducens nerve and related disorders pave the way for innovative treatment modalities. Pioneering techniques, including neurostimulation and neuroregeneration therapies, hold promise for individuals with abducens nerve-related impairments. However, further research and clinical trials are necessary to validate the efficacy and safety of these emerging treatment approaches.
Neurostimulation involves the use of electrical impulses to modulate the activity of the abducens nerve or its associated neural networks. By precisely targeting specific regions of the brain involved in eye movement control, researchers aim to restore normal function in individuals with abducens nerve palsy. This approach has shown encouraging results in preliminary studies, with some patients experiencing improved eye movement and reduced diplopia (double vision).
Neuroregeneration therapies, on the other hand, focus on promoting the regrowth and repair of damaged abducens nerve fibers. Various experimental approaches, such as stem cell transplantation and gene therapy, are being explored to stimulate nerve regeneration and restore proper connectivity. These cutting-edge techniques hold the potential to revolutionize the treatment of abducens nerve disorders, offering hope for individuals with long-standing impairments.
In conclusion, recent research on the abducens nerve has brought about significant advancements in our understanding of its function and associated disorders. The use of advanced imaging techniques, such as MRI and DTI, has provided valuable insights into the structural and functional aspects of the abducens nerve. Furthermore, innovative treatment modalities like neurostimulation and neuroregeneration therapies show promise in improving the lives of individuals with abducens nerve-related impairments. Continued research in this field will undoubtedly lead to further breakthroughs and a deeper understanding of the intricate workings of the ocular motor system.
Conclusion
In conclusion, the abducens nerve’s termination point lies within the lateral rectus muscle, enabling it to exert control over this vital structure responsible for outward eye movements. Understanding the anatomy, function, pathway, and disorders related to the abducens nerve allows healthcare professionals to diagnose and manage patients more effectively. Recent advancements in the field of neurology offer hope for enhanced diagnosis, treatment, and potential future interventions. If you or someone you know experiences symptoms related to the abducens nerve, it is crucial to seek medical advice and explore appropriate treatment options to optimize recovery and ensure optimal ocular motor function.
Leave a Reply