Cranial nerve VI, also known as the abducens nerve, is a vital component of the human nervous system. As one of the twelve cranial nerves, it plays a crucial role in the innervation of the eye muscles responsible for lateral eye movement. Understanding the function, anatomy, pathway, clinical significance, and treatment of the abducens nerve is essential for medical professionals and those interested in the intricacies of the human body.
Understanding the Function of Cranial Nerve VI
The abducens nerve, also known as cranial nerve VI, plays a crucial role in eye movement. It is primarily responsible for the lateral movement of the eye, a process known as abduction. This essential function allows the eyes to move laterally, facilitating effective scanning of the environment and enabling binocular vision.
When we look around, our eyes need to move in different directions to focus on different objects. The abducens nerve innervates the lateral rectus muscle, which acts as an antagonist to the medial rectus muscle innervated by the oculomotor nerve. The balanced interplay between these two muscles allows for lateral and medial eye movements, respectively.
Imagine trying to look at an object on your right side without the ability to move your eyes laterally. It would be challenging to scan your surroundings, read, or even drive a car. Dysfunction of the abducens nerve can severely impact eye coordination and visual acuity, leading to a condition known as abducens nerve palsy.
Role of the Abducens Nerve in Eye Movement
The abducens nerve plays a vital role in coordinating eye movements. It works in conjunction with other cranial nerves to ensure smooth and precise eye motion. When the abducens nerve is functioning correctly, it allows us to effortlessly shift our gaze from one point to another, enhancing our visual perception and spatial awareness.
Imagine watching a tennis match without the ability to move your eyes laterally. You would struggle to follow the ball as it moves from one side of the court to the other. The abducens nerve enables us to track moving objects, making activities like playing sports or watching action-packed movies more enjoyable.
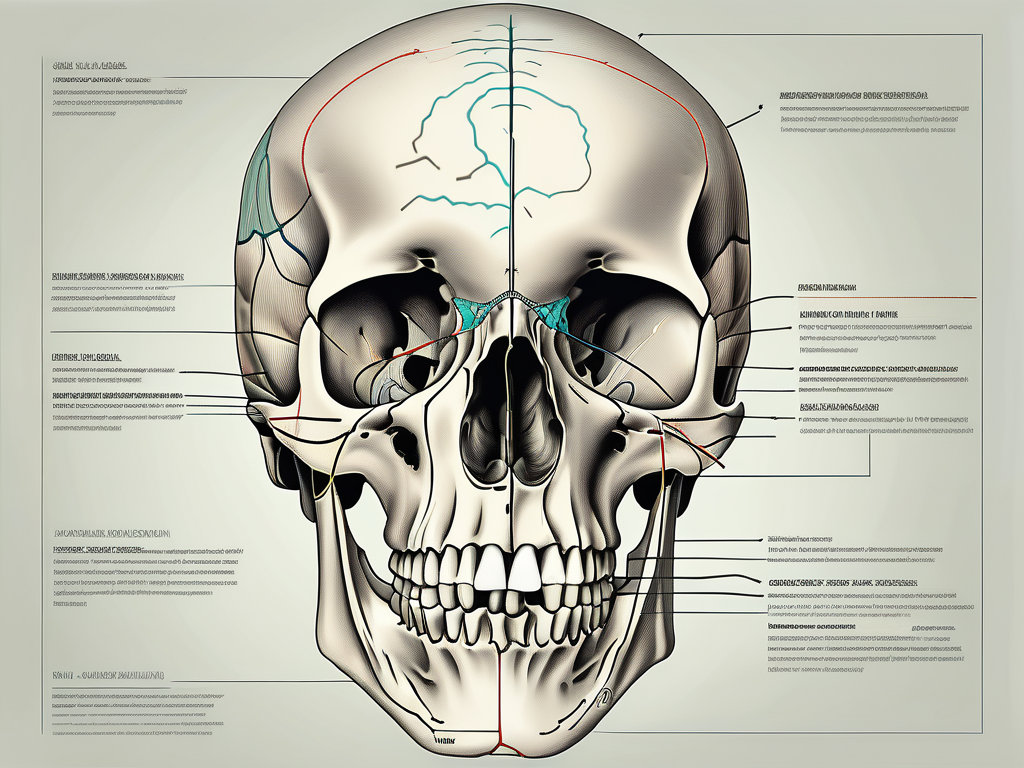
Anatomy of the Abducens Nerve
The abducens nerve originates in the pons region of the brainstem, a critical part of the central nervous system. Emerging from the brainstem, it traverses its course towards the cavernous sinus, an important venous structure located within the skull.
The path of the abducens nerve within the cavernous sinus is fascinating. It runs in close proximity to other vital cranial nerves and blood vessels, creating a complex network of neural and vascular structures. This intricate arrangement makes the abducens nerve susceptible to compression and injury.
Various factors, such as tumors, infections, or trauma, can exert pressure on the abducens nerve, leading to its dysfunction. Understanding the anatomy of the abducens nerve helps us appreciate the delicate nature of this structure and the importance of its proper functioning.
Pathway of the Abducens Nerve through the Cranium
Understanding the precise pathway of the abducens nerve through the cranium is crucial in diagnosing and managing potential disorders related to this cranial nerve.
The abducens nerve, also known as the sixth cranial nerve, plays a vital role in eye movement. It is responsible for the lateral movement of the eye, allowing us to look to the side.
Origin and Course of the Abducens Nerve
The abducens nerve originates from the abducens nucleus, which lies within the pons of the brainstem. This nucleus is located in the lower part of the pons, near the midline. From there, the nerve fibers of the abducens nerve travel a long and intricate path to reach their final destination.
Once the nerve fibers leave the abducens nucleus, they pass through the pontine tegmentum, a region of the brainstem that contains various important structures involved in motor control and sensory processing. As the nerve fibers continue their journey, they enter the subarachnoid space, a fluid-filled space that surrounds the brain and spinal cord.
From the subarachnoid space, the abducens nerve fibers enter the cavernous sinus, a large venous sinus located on each side of the sella turcica, a bony structure in the middle cranial fossa. The cavernous sinus is a complex network of veins and serves as a pathway for several cranial nerves and blood vessels.
As the abducens nerve traverses through the cavernous sinus, it comes into close proximity with important structures such as the internal carotid artery and the ophthalmic artery. These arteries supply blood to the brain and the eye, respectively. The close relationship between the abducens nerve and these blood vessels is significant, as any pathology affecting these vessels can potentially impact the function of the abducens nerve.
After passing through the cavernous sinus, the abducens nerve exits the skull through a small opening called the superior orbital fissure. This fissure is located in the sphenoid bone, one of the bones that make up the orbit, or eye socket. Once inside the orbit, the abducens nerve innervates the lateral rectus muscle, which is responsible for the abduction of the eye.
Key Structures Along the Pathway
During its pathway through the cranium, the abducens nerve comes into close proximity with several important structures. These include the internal carotid artery, ophthalmic artery, and other cranial nerves such as the oculomotor, trochlear, and trigeminal nerves. Understanding the relationships between these structures is crucial for diagnosing and treating disorders associated with the abducens nerve.
The oculomotor nerve, which is responsible for the movement of most of the extraocular muscles, lies adjacent to the abducens nerve within the cavernous sinus. The trochlear nerve, which controls the superior oblique muscle, also passes through the cavernous sinus in close proximity to the abducens nerve. The trigeminal nerve, a major sensory nerve of the face, also travels through the cavernous sinus and may interact with the abducens nerve along its pathway.
Disorders affecting the abducens nerve can result in a condition known as abducens nerve palsy, characterized by the inability to move the affected eye laterally. This can lead to double vision and difficulty in focusing on objects to the side. Common causes of abducens nerve palsy include trauma, infections, tumors, and vascular disorders affecting the blood supply to the nerve.
In conclusion, the pathway of the abducens nerve through the cranium is a complex and intricate journey. Understanding this pathway and the relationships between the abducens nerve and other structures is essential for diagnosing and managing disorders related to this important cranial nerve.
Clinical Significance of the Abducens Nerve
The abducens nerve’s clinical significance extends to various disorders that can affect its functionality and cause significant visual impairments.
The abducens nerve, also known as the sixth cranial nerve, plays a crucial role in eye movement. It innervates the lateral rectus muscle, which is responsible for the abduction of the eye, allowing it to move laterally away from the midline. Any disruption in the functioning of this nerve can lead to debilitating conditions and impact a person’s quality of life.
Common Disorders Involving the Abducens Nerve
Abducens nerve palsy is a prevalent disorder affecting the functioning of the abducens nerve. It can result from various causes, including trauma, tumors, infections, and vascular abnormalities. The resulting inability to abduct the eye can lead to double vision, reduced depth perception, and challenges in daily activities.
Another disorder that can affect the abducens nerve is internuclear ophthalmoplegia (INO). INO is characterized by impaired adduction of the eye on the affected side and nystagmus in the abducting eye. It is often associated with neurological conditions such as multiple sclerosis.
Additionally, abducens nerve compression can occur due to aneurysms or tumors in the vicinity of the nerve. This compression can lead to symptoms such as diplopia (double vision), headaches, and facial pain.
Diagnostic Techniques for Abducens Nerve Damage
Accurate diagnosis of abducens nerve disorders is essential for effective management. Physicians employ various diagnostic techniques such as thorough medical history assessments, complete neurological examinations, and specialized imaging studies like magnetic resonance imaging (MRI) and computed tomography (CT) scans.
During a medical history assessment, the physician will inquire about symptoms, their duration, and any associated factors. They will also evaluate the patient’s medical history for any underlying conditions or previous trauma that could contribute to the nerve dysfunction.
A complete neurological examination is crucial for assessing the function of the abducens nerve. This examination may involve assessing eye movements, checking for nystagmus, and evaluating the strength and coordination of the eye muscles.
In cases where further imaging is required, magnetic resonance imaging (MRI) and computed tomography (CT) scans can provide detailed images of the brain and surrounding structures. These imaging studies can help identify any structural abnormalities, such as tumors or vascular malformations, that may be causing the abducens nerve dysfunction.
Consulting a medical professional is crucial for accurate diagnosis and tailored treatment plans. Early detection and intervention can significantly improve the prognosis and quality of life for individuals with abducens nerve disorders.
Treatment and Management of Abducens Nerve Disorders
Efficient management of abducens nerve disorders requires a comprehensive approach that addresses the underlying cause and provides symptomatic relief. The abducens nerve, also known as cranial nerve VI, is responsible for the innervation of the lateral rectus muscle, which controls the movement of the eye away from the midline. When this nerve is affected, it can lead to a condition known as abducens nerve palsy, causing difficulties in eye movement and coordination.
Therapeutic Approaches for Abducens Nerve Palsy
Treatment options for abducens nerve palsy aim to correct the underlying cause, if possible, and improve eye movements. Depending on severity and etiology, treatment may involve conservative approaches, such as patching the unaffected eye to promote visual strengthening, or surgical interventions to correct muscle abnormalities or alleviate compression. In some cases, medications may be prescribed to manage symptoms and reduce inflammation.
Additionally, physical therapy and occupational therapy can play a crucial role in the management of abducens nerve palsy. These therapies focus on strengthening the eye muscles, improving coordination, and enhancing overall visual function. Through a combination of exercises, visual stimulation, and specialized techniques, individuals with abducens nerve palsy can regain control over their eye movements and improve their quality of life.
Rehabilitation and Recovery from Abducens Nerve Damage
Rehabilitation programs focused on eye coordination exercises and visual therapies can be beneficial for individuals experiencing abducens nerve damage. These programs aim to enhance eye movement capabilities, improve binocular vision, and enhance overall quality of life. Consulting with a medical professional experienced in neurology or ophthalmology is crucial in establishing an appropriate rehabilitation plan.
Furthermore, it is important to address any underlying medical conditions that may contribute to abducens nerve damage. Conditions such as diabetes, hypertension, and autoimmune disorders can affect the health of the nerves and exacerbate symptoms. By managing these conditions effectively, individuals can improve their chances of recovery and minimize the risk of further nerve damage.
In conclusion, cranial nerve VI, or the abducens nerve, plays a vital role in eye movement and coordination. Understanding the function, anatomy, pathway, clinical significance, and treatment options related to this important cranial nerve is imperative for healthcare professionals and those affected by abducens nerve disorders. If you suspect any issues related to the abducens nerve or experience visual impairments, it is essential to consult with a qualified medical professional who can provide accurate diagnosis and guidance for individualized treatment and management plans.
Leave a Reply